Repairing the World by Repairing Women’s Bodies in Rwanda and Niger
Barbara A. Margolies, founder and executive director of the International Organization for Women and Development (IOWD), believes in personal reinvention. The former elementary school teacher-turned-children’s-book-author has, since 2003, brought groups of U.S. volunteers—most of them doctors and registered nurses—to treat women suffering from a host of reproductive health problems, including obstetric fistula.

In Rwanda, repaired patients giving Barbara Margolies gifts at a Day of Dignity celebration.
Margolies, never intended to be involved in healthcare delivery, but, she says, “if you keep the doors open and push through them, you never know what you’ll find.”
In her case, the doors led to the landlocked country of Niger, a former French colony and the largest country in West Africa. Margolies visited Niger for the first time in 2001 as part of a two-week mission, sponsored by the U.S. State Department, to teach English classes to educators. Several successive teaching stints followed this initial foray and, over time, Margolies and the State Department’s Public Affairs Director in Niger became acquainted. What followed were introductions to numerous high-level officials, including the country’s minister of health, who asked Margolies if she could help the nation improve its healthcare systems.
“My husband and I had given financial support to Health Africa (AMREF), an African medical relief organization, and I introduced Niger’s Minister of Health to AMREF and to several other U.S.-based non-governmental organizations,” Margolies begins. “After some discussion, AMREF agreed to send a doctor to Niger to assess the country’s health needs.” The assessment took place in 2002 and the findings shocked Margolies.
“He told me that there were 80 women living in the courtyard of the National Hospital, sleeping on mattresses on a cement floor. They were there because they had obstetric fistula and had nowhere else to stay. Some had been there for 20 years. These women could no longer contain their bodily wastes and even though they put their mattresses in the sun to dry each morning, he said the stench was overwhelming.”
Margolies admits that she knew absolutely nothing about obstetric fistula when she heard this account. She was both intrigued and horrified, and wanted to know more about the condition and its treatment, so as soon as she returned to the U.S. She contacted her gynecologist and asked a slew of questions. What she learned, she says, was eye-opening.
Obstetric fistula, she discovered, are holes between the vagina and rectum that develop during a long, obstructed labor as the baby tries to emerge. In addition to the fact that the baby may not survive the difficult birth, the damage to her tissue leaves the woman leaking urine, feces, or both. The condition, common in the poorest parts of Asia and sub-Saharan Africa, is estimated by the World Health Organization to impact two million women, with between 50,000 and 100,000 new cases diagnosed annually. The World Health Organization calls obstetric fistula “the untreated tragedy.” Even more troubling, Margolies learned that fistula can be prevented by access to timely and hygienic Cesarean sections. Most shocking, if a fistula does occur, it can often be repaired by a surgical procedure.
There were 80 women living in the courtyard of the National Hospital, sleeping on mattresses on a cement floor. They were there because they had obstetric fistula and had nowhere else to stay. These women could no longer contain their bodily waste. The stench was overwhelming.
Margolies found this information enraging. “When my doctor explained what fistulas are and why they occur, I had just one question: How do we help?” Margolies recalls. “To be aware that women live like this blew me away. I never thought I’d do anything like this. I had not been part of feminist organizing in the 1970s or 80s and had always danced to my own tune. But when I learned about fistula, I knew I had to reach out and do something about them.”
Margolies’s first step was to contact Urogynecologist/Pelvic Floor Reconstructive Surgeons—a small, New York-area group that her doctor suggested to her. She described what she’d learned to the staff and her conversation paid off; in short order, she persuaded the practice to act. In December 2003, the group sent four female surgeons to Niger for 10 days. The 80 women living in the hospital courtyard were the first people they evaluated. “Some were beyond help,” Margolies says, “but the doctors did what they could to repair the damage for as many women as they could.”
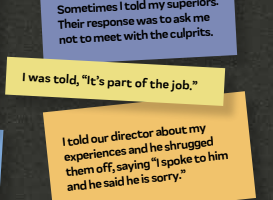
It was a difficult trip, made harder by the blatant sexism the team had to contend with. “The doctors and hospital workers in Niger had never seen a woman surgeon, and their backs initially went up when we arrived,” Margolies continues. “They eventually apologized when they realized that these doctors were very good at what they did.”
Indeed, by the end of the visit, everyone was calling the venture a success and expressed interest in repeating it, so Margolies shelled out $10,000 of her own money to incorporate as the International Organization for Women and Development. She also pulled together a board of directors and paid lawyers to help the fledgling organization apply for tax-exempt status. Since then, she laughs, “my family and friends have been very generous.”
So have the several hundred medical personnel who have volunteered with IOWD, all of whom pay their own way—approximately $2500 for travel, hotels, and food for their 14-day stay—and typically use their vacation time to participate in the project. In fact, Margolies says that the group’s $100,000 yearly budget is extremely tight and goes to cover the purchase and shipping of equipment and supplies—monitors, sutures, and medications—necessary to treat their patients, none of whom pay for the examinations, surgery or recuperative care they receive.
Still, as you’d expect, the work has not been without operational challenges and frustrations. Now in its 15th year, the IOWD can no longer work in Niger; despite 29 successful trips to perform fistula repair, by 2009 political instability made travel there unsafe, so Margolies had to find another country in which to work.
The organization currently operates in Rwanda, where teams of IOWD volunteers spend a total of six weeks a year—two weeks at a time in January, May, and October—attending to patients. Some of the volunteers come repeatedly, while others volunteer just once. While in Rwanda, they work in Kibagabaga Hospital in Kigali, the country’s capital city, where they do a host of things. In addition to fistula repair, doctors fix botched C-sections and perform hysterectomies, cancer surgeries, and screenings. They also do follow-up and aftercare. But regardless of the task, it is service, rather than charity work or philanthropy, that lies at the core of IOWD activities.
Dr. Joshua Holden has been going to Rwanda with this organization since 2010. An obstetrician-gynecologist at New York’s Columbia University Medical Center, Holden first learned about the organization from a colleague who’d gone on several IOWD missions and gave a talk about his experience. His coworker’s stories, Holden says, inspired him. When he returned home and told his wife what he’d heard, she announced, “You have to go.”
And although Holden has a great deal of technical know-how, and performs a small number of surgeries during each trip to Rwanda, his primary task now is that of educator, teaching physicians and medical students best practices to avoid fistula, oversee safer deliveries, and perform successful C-sections. This work is essential, he says, since training the next generation of physicians is imperative for the nation’s development.
The facts speak for themselves. Margolies reports that 48 percent of the women the IOWD now treats developed fistula because of C-section complications—not because of prolonged labor—which makes this an urgent and growing concern for the country’s women. The reason is prevalence. As the U.S. National Library of the National Institutes of Health reports, C-sections presently account for 15 per-cent of the deliveries in Rwanda. “High cesarean delivery rates may lead to an increase in maternal morbidity and mortality, as C-sections are associated with a 5-fold to 20-fold increased rate of infection compared to vaginal deliveries,” the NIH warns.
People ask me how a Jewish grandmother from Rockville Centre, New York, came to do this. For me, it’s about fixing something that can be fixed.
Understanding that education is key to improving maternal health care, Margolies’s organization wants to make sure that Rwanda’s physicians get the training they need to function without outside assistance, no matter how generous, helpful, or well-meaning it is. “We’re working with the Minister of Health to create a curriculum—complete with a step-by-step video—that shows the proper techniques for C-sections,” Holden says. “It also deals with how best to treat things like parasites and worms that the patient may present with. The curriculum discusses when and why to prescribe antibiotics and shows the doctor or student how to clean a patient properly to avoid infection.”
Although implementing the finalized curriculum in Rwandan medical schools has been slower than Holden would like, he notes that the hands-on training has been wonderfully received. “The medical students and young attending physicians appreciate our time and energy, and have tons of questions, but the frustration is that we typically reach only a small number of people, two to 10 doctors per cycle. This means that my work as a teacher is very different from what I did as part of a fistula team. That work was immediately gratifying. We’d treat 150 patients, 90 percent of whom were cured by the time we left the country.”
Holden plans to return to Rwanda in May, though he concedes that he sometimes feels his work there is a drop in the proverbial bucket. “It’s hard not to feel like we’re spinning our wheels,” he says, especially when equipment gets broken or when there are administrative or bureaucratic roadblocks.
So why do you keep returning? I ask. “People in Rwanda understand that pregnancy is risky and aging is inevitable. Death is simply a part of life in Rwanda.” Even when a child does not survive, people are grateful for the care they received, something that allows them to move on, despite their grief and mourning. “They have faith that they’ll be reunited with their child when they get to heaven,” Holden says. “Furthermore, Rwandans understand that not everyone can be cured. Sometimes you just need to take an elder home and care for them until they die. It’s humbling to learn from them and get to know their point of view.”
It’s also often life-changing for both the patients and the volunteers who take part in these programs. “Providing surgical care allows us to change people’s lives, one woman at a time,” Barbara Margolies concludes. “To not stink anymore and be able to socialize, go to church, or go shopping for themselves is incredible. IOWD has taken 54 trips to Africa—Niger and Rwanda combined—and it never gets tired.
“People ask me how a Jewish grandmother from Rockville Centre, New York, came to do this. For me, it’s about fixing something that can be fixed. In addition, I see the Rwandan genocide of the Tutsi, which ended in 1994 and led to more than 800,000 deaths, as very much like the Nazi Holocaust. I related to it immediately and I wanted to help the country recover. There are so many needs that we, as individuals, can address.… I know that this is not possible for everyone, but I went from teaching, to writing books, to running IOWD. Everyone can do something useful if they want to.”
Eleanor J. Bader is a Brooklyn, NY-based teacher at Kingsborough Community College/CUNY and an award-winning freelance writer.