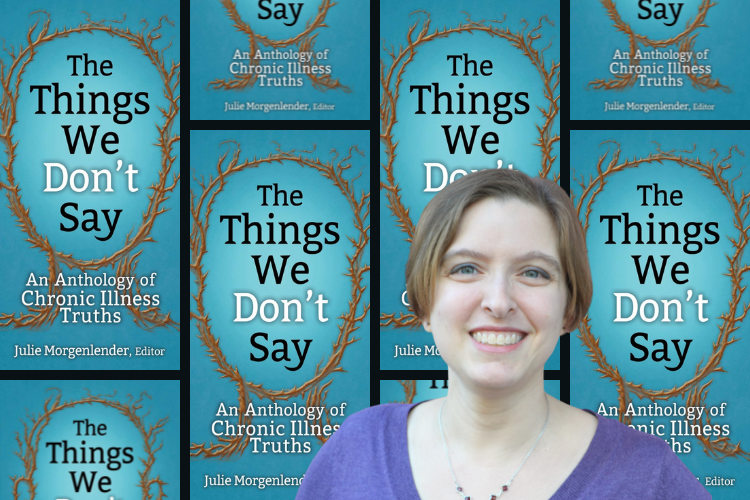
The Things We Don’t Say: An Interview with Julie Morgenlender
Since childhood, Julie Morgenlender has been living with chronic illness. From trying to prove to doctors it wasn’t all in her head, to fighting with insurance to cover essential medical treatments, to curtailing her career, Morgenlender has lived through it all. Enlightening and powerful, The Things We Don’t Say: An Anthology of Chronic Illness Truths, chronicles some of her experiences alongside essays from a diverse group of people from around the world living with chronic illness. Here, Morgenlender talks to Hanna R. Neier about finding community, medical gender bias, and how a little Jewish compassion can go a long way.

HN: Your story alone could have made a great memoir. Why create an anthology instead?
JM: I wanted to provide a sense of community. People with chronic illnesses often feel isolated and face a lack of understanding from others. We often feel like we’re the only ones dealing with our issues. By bringing together so many voices, I hope that every reader can find at least one author, one story, with which they can identify. I also wanted this book to help loved ones gain a better understanding of what we live with, so sharing multiple stories highlights that this isn’t just one person’s experience.
How did you choose the essays?
My goals were variety and diversity, again with the hope that this would show the range of our experiences and help people find connection. I wanted an array of subjects, from medical situations to family relationships to stigmas we face. I wanted authors of different ages, races, and gender identities who had different symptoms and diagnoses. There was no way to cover every intersectional identity or every diagnosis, but the book touches on many of them.
We Jews joke a lot about Jewish guilt which tends to come from external sources—like a family member using guilt to get a desired result. By contrast, chronic illness guilt is internal.
At sixteen you were in pain, but your doctors sent you to a psychologist, claiming you were looking for attention. One of your authors had a similar experience. She explains this is common amongst women.
Gender bias in medical care is a known problem. Considering the sexism that is so prevalent in our society, it’s not surprising, but still upsetting. (To my knowledge, there haven’t been studies about sexism in the treatment of non-binary or transgender patients.) Men are often taken more seriously when they seek care for the same symptoms for which women are dismissed. If a cause of symptoms isn’t clear, too often women are told we’re imagining our problems. I have no way of knowing if I would have been taken more seriously if I had been a man, but I have my suspicions.
You write that you grew up with Jewish guilt, but that chronic illness guilt is much worse. Can you elaborate?
We Jews joke a lot about Jewish guilt which tends to come from external sources—like a family member using guilt to get a desired result. By contrast, chronic illness guilt is internal. There’s a lot of frustration and self-reproach that comes out of not being able to meet seemingly reasonable expectations like keeping a date or a promise. Because the cause is within us—within our own bodies—it feels like it should be under our control, but it’s not.
The pandemic has created a lot of shifts in our society, most notably work-from-home arrangements. How has this benefited people with chronic illness? Do you think it will push employers in the future to be more accommodating?
Many disabled employees were denied requests to work from home before the pandemic. When entire offices were sent home, they finally received the accommodations they needed. Now as offices reopen, workers are again being denied requests to continue working from home. Luckily, some offices are planning to offer remote work on an ongoing basis, which benefits disabled workers. But in both cases, people who need accommodations are just expected to go along with office protocol. Obviously, there are exceptions. I hope that employers will take note of how well remote work functioned and be more accommodating to disabled employees in the future, including the many more people who might develop chronic illnesses due to COVID-19’s long-term effects. But without the proper laws in place (and this doesn’t seem to be changing any time soon) these accommodations will be far too arbitrary.
And let’s remember the many people who were at higher risk of COVID-19 complications who were denied accommodations. Teachers, grocery store workers, and others were told they must show up in person to work. If we are to judge a society by how it treats its most vulnerable, then I believe we were failing before the pandemic, and though a light has been shined on the issue, nothing has really changed.
In Judaism, the preservation of human life takes precedence: Jews are exempt from fasting on Yom Kippur, standing for the Torah, etc. if it is threatening to their health. Thoughts?
I love how accommodating Judaism is, in ways that too often the rest of society isn’t. Our culture has survived for many years while allowing rules to be bent and broken when necessary. There is so much we could do for others by modeling that same kind of compassion: being kind when someone requests substitutions in restaurants, letting more people work from home, and broadening insurance coverage for better medical care.
The book has garnered a lot of attention especially in the chronic illness community. How do you feel about that?
While I’m not surprised that people have connected deeply with the stories, I was still caught off-guard by just how much it resonates. I have received so much amazing feedback in the year since the book came out, from folks with chronic illness who feel less alone and from loved ones who say they better understand what their family and friends are living with, and even some doctors who say they can better understand their patients. It has been humbling and rewarding.